GAD antibodies in neurological disorders insights and challenges
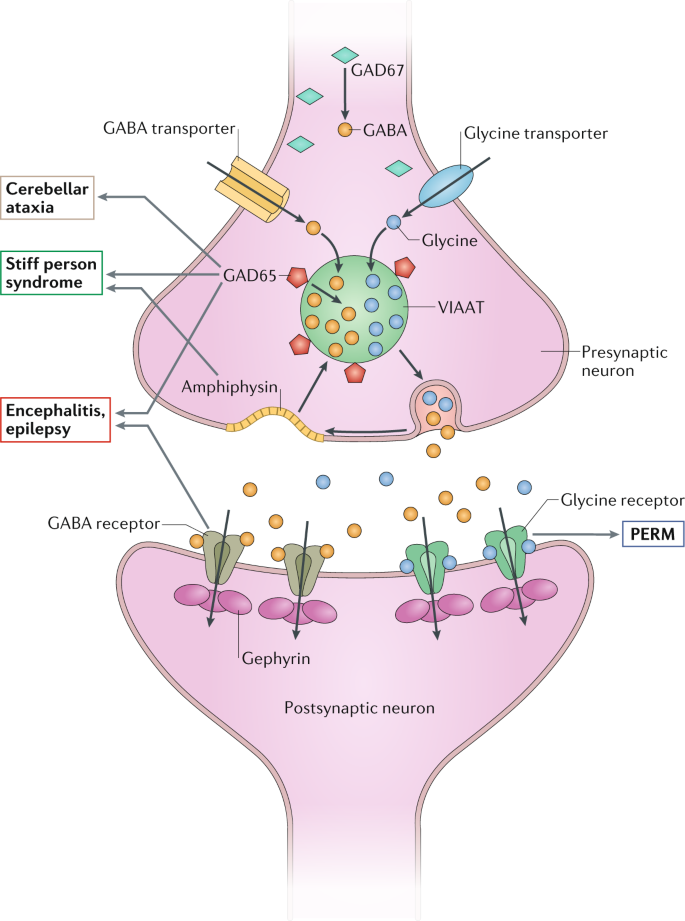
Antibodies to glutamic acid decarboxylase (GAD) have been associated with several neurological syndromes, including stiff-person syndrome, cerebellar ataxia and epilepsy. These antibodies were first described in 1988, but several controversies about GAD autoimmunity still remain.
No criteria exist to establish when a neurological syndrome is pathogenically linked to GAD antibodies, often leading to the assumption that any syndrome in which these antibodies are present is immune mediated, sometimes resulting in misdiagnosis and unnecessary treatment.
In this Review, we provide recommendations for assessing the association between a neurological syndrome and the presence of GAD antibodies, and we critically review the evidence on the pathogenicity of GAD antibodies. Given that stiff-person syndrome is usually autoimmune, the presence of GAD antibodies in the cerebrospinal fluid is sufficient to confirm a pathogenic link with GAD autoimmunity.
However, for cerebellar ataxia, epilepsy and other syndromes with different aetiologies, we propose that confirmation of a pathogenic link with GAD autoimmunity requires demonstration of intrathecal GAD antibody synthesis. Nevertheless, the evidence that GAD antibodies are directly pathogenic is not yet convincing. Studies in animal models are needed to demonstrate whether neurological syndromes are directly caused by specific disruption of GAD function by GAD antibodies.
Key points
-
The main neurological syndromes associated with high levels of antibodies to glutamic acid decarboxylase (GAD) include stiff-person syndrome, cerebellar ataxia and temporal lobe epilepsy.
-
Serum levels of GAD antibodies can be considered high when quantitative tests (radioimmunoassays or enzyme-linked immunosorbent assays) and qualitative tests (immunohistochemistry, cell-based assays or line-blot assays) are positive.
-
Cerebrospinal fluid levels and intrathecal synthesis of GAD antibodies should be determined in all patients with suspected CNS syndromes and high serum levels of GAD antibodies.
-
We propose that the diagnosis of probable or definite GAD antibody-associated syndrome must be based on the spectrum of symptoms, serum levels of GAD antibodies and demonstration of intrathecal antibody synthesis.
-
There is no clear evidence that GAD antibodies are pathogenic in any of the associated CNS syndromes (stiff-person syndrome, cerebellar ataxia, temporal lobe epilepsy or limbic encephalitis).
-
In general, immunotherapy has limited effects on the outcomes of neurological syndromes associated with GAD antibodies.